Central venous access devices (CVADs) are vital components in modern medical care, commonly used for patients requiring long-term intravenous therapy. These devices serve critical roles in facilitating the administration of medications, nutrition, and other therapeutic agents directly into the patient’s bloodstream, bypassing peripheral venous routes. Given their importance in delivering lifesaving treatments, understanding CVADs, their applications, and management is crucial for healthcare professionals and stakeholders involved in patient care.
Read Now : Tailored Treatment Through Genomics
Types of Central Venous Access Devices
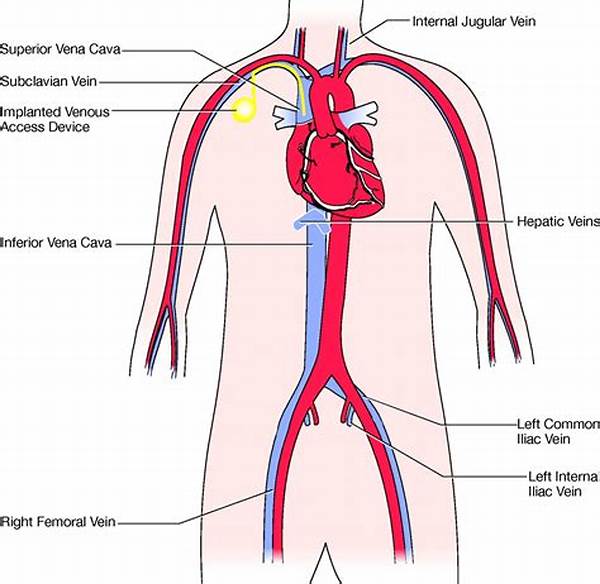
There are several types of central venous access devices, each designed to meet specific medical needs. The primary types include tunneled catheters, peripherally inserted central catheters (PICCs), and implanted ports. Tunneled catheters are usually inserted into a large vein near the neck or chest and are intended for long-term use. PICCs are inserted into veins in the arm and are typically preferred for medium- to long-term treatments. Implanted ports, on the other hand, are placed under the skin, providing a more discreet option for patients needing intermittent access. Each type has its advantages and specific use cases, and the selection of a CVAD depends on various factors, including the anticipated duration of treatment, patient preference, and clinical indications. The role of healthcare professionals in determining the most appropriate CVAD for individual patients is vital to ensure optimal outcomes and comfort.
Insertion and Maintenance of Central Venous Access Devices
The insertion of central venous access devices requires careful planning and precision. The procedure is often performed under sterile conditions to minimize the risk of infection. Healthcare professionals, particularly those trained in central line placement, are responsible for the insertion process. Once successfully placed, CVADs require regular maintenance to ensure functionality and to prevent complications such as infection or thrombosis. Cleaning protocols, regular flushing, and diligent observation for any signs of infection are critical components of CVAD maintenance. Effective management of these devices is imperative for patient safety and the delivery of seamless healthcare services, underscoring the significance of specialized training and adherence to established clinical guidelines.
Advantages of Central Venous Access Devices
1. Long-term Therapy: Central venous access devices allow for the administration of medications over prolonged periods without repeated needle sticks, making them ideal for long-term treatments.
2. Patient Comfort: These devices offer enhanced patient comfort by reducing the need for peripheral venipuncture, leading to less pain and discomfort.
3. Efficient Delivery: CVADs enable the efficient delivery of higher volumes of fluids and medications, crucial for patients requiring rapid interventions.
4. Multiple Uses: They facilitate the concurrent administration of various drugs, nutrition, and blood products, optimizing treatment efficiency.
5. Minimized Complications: CVADs minimize the risk of extravasation by delivering substances directly into large central veins, thus reducing the incidence of complications associated with peripheral infusions.
Read Now : Data Security In Healthcare Solutions
Potential Complications
Despite their benefits, central venous access devices are not without risks. Complications may include infection, thrombosis, or mechanical issues necessitating prompt attention. Infection remains the most significant concern, given its potential to lead to severe systemic effects. Thrombosis, or the formation of blood clots, may obstruct the catheter, leading to its dysfunction or requiring intervention to dissolve or remove the clot. Mechanical complications, such as kinking or dislodgement of the device, may impact its effectiveness, requiring careful monitoring and interventions by healthcare providers. It is essential to recognize and manage these complications promptly to maintain the efficacy and safety of central venous access devices for patient care.
Monitoring and Care of Central Venous Access Devices
The ongoing monitoring and care of central venous access devices are paramount to ensuring optimal patient outcomes. Regular assessment by healthcare professionals involves inspecting the insertion site for signs of infection, such as redness, swelling, or discharge. Additionally, the catheter’s patency is checked to confirm that it remains open and functional, allowing uninterrupted administration of medications and fluids. Patient education plays a crucial role in the successful management of CVADs, with individuals and their caregivers receiving training on proper care techniques and early warning signs of potential complications. This collaborative approach empowers patients and supports healthcare teams in delivering effective and safe therapeutic interventions.
Innovations and Future Directions
Advancements in central venous access devices and their management continue to evolve, driven by the need for safer and more efficient patient care solutions. New materials and technologies aimed at reducing infection rates and improving the ease of use are under active development. Furthermore, innovations in imaging and placement techniques are enhancing the precision and success rates of CVAD insertions. As research progresses, the focus remains on improving patient comfort and minimizing complications, highlighting the dynamic nature of healthcare technology and its potential to redefine treatment paradigms.
Conclusion
In summary, central venous access devices are integral to the delivery of modern healthcare, providing essential benefits for patients requiring long-term and complex medical therapies. Understanding the various types, advantages, and potential complications of CVADs is crucial for healthcare providers to ensure patient safety and treatment efficacy. Through continuous advancements and diligent care practices, central venous access devices will continue to play a pivotal role in improving patient outcomes and quality of life in diverse clinical settings.