In the realm of healthcare, the meticulous prescribing of medication stands as a crucial pillar for ensuring patient safety and efficacious treatment outcomes. The complexity of hospital environments, coupled with the diverse array of medications available, necessitates adherence to best practices for hospital medication prescribing. These practices are essential for minimizing errors, enhancing therapeutic benefits, and safeguarding patient wellbeing. Fundamentally, the goal is to provide precise, appropriate, and individualized medication therapies, reinforcing the significance of evidence-based protocols.
Read Now : Long-term Drug Therapy Implications
Importance of Best Practices in Prescribing
The implementation of best practices for hospital medication prescribing ensures the delivery of safe and effective healthcare. Given the intricate nature of healthcare systems, it is imperative for medical professionals to adhere to standardized practices that foster consistency and accuracy. Effective prescribing encompasses the thorough assessment of patient histories, careful consideration of potential drug interactions, and the tailoring of dosage regimens to individual patient needs. Moreover, the integration of technology, such as electronic prescribing systems, has become indispensable in minimizing human errors and enhancing the overall efficiency of the prescribing process. By adhering to best practices for hospital medication prescribing, healthcare providers can significantly reduce adverse drug events, ultimately fostering better patient outcomes and heightened trust in the healthcare system.
In addition, continuous education and training for healthcare professionals play a vital role in reinforcing best practices for hospital medication prescribing. Staying abreast with the latest developments in pharmacology and integrating contemporary research findings into practice helps ensure that medical staff can make informed decisions that prioritize patient safety. Furthermore, the cultivation of a collaborative environment involving pharmacists, nurses, and physicians is crucial. This multidisciplinary approach facilitates comprehensive medication management and promotes a culture of safety, allowing for real-time consultations and knowledge sharing that further minimize risks. Collectively, the conscientious observance of best practices for hospital medication prescribing serves as a cornerstone for delivering high-quality care.
Key Components of Effective Prescribing
1. Patient Assessment: The foundation of best practices for hospital medication prescribing lies in a thorough patient evaluation. Understanding patient history, allergies, and current conditions is vital for appropriate medication selection.
2. Drug Interaction Awareness: Being vigilant about potential drug-drug interactions is integral. Best practices for hospital medication prescribing mandate careful analysis of all medications a patient is currently taking.
3. Dosage Accuracy: Accurate dosing is crucial in best practices for hospital medication prescribing to avoid under-treatment or adverse effects from excessive dosages.
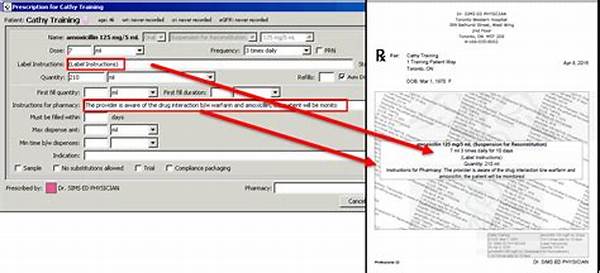
4. Use of Technology: Implementing electronic prescribing systems significantly reduces errors, showcasing the importance of integrating technology into best practices for hospital medication prescribing.
5. Interdisciplinary Collaboration: Engaging pharmacists, doctors, and nurses in medication management exemplifies best practices for hospital medication prescribing, promoting a holistic approach to patient care.
Technological Advancements in Prescribing
Technological innovations have revolutionized the landscape of hospital medication prescribing, providing a robust framework for maintaining high standards of patient care. At the forefront of these innovations are electronic prescribing systems, which form a core component of best practices for hospital medication prescribing. These systems offer a host of advantages, including real-time access to patient records, comprehensive drug databases, and integrated decision-support tools. Such features are instrumental in reducing prescription errors and enhancing the precision and reliability of medication management. Furthermore, the seamless integration of these systems with other hospital information systems ensures a cohesive flow of information, thus supporting effective communication among healthcare providers.
Advanced technology also facilitates the monitoring and evaluation of prescribing patterns, allowing for the identification of areas in need of improvement. By implementing data analytics and tracking tools, hospitals can ensure adherence to guidelines and adjust practices based on emerging trends and evidence-based research. The evolving landscape of digital health presents an opportunity to further embed these tools within the framework of best practices for hospital medication prescribing, thereby optimizing the quality of patient care. Central to this transformation is the need for continued investment in training and infrastructure to support the widespread adoption of such technologies across healthcare institutions.
Best Practices Explained Casually
1. Patient Checkin’: Know the deets about your patients ’cause it’s all about finding the right meds that won’t mess them up.
2. Mix & Match No-Go: Don’t just toss meds together. Best practices for hospital medication prescribing means knowing which ones play nice.
3. Dose It Right: Not too much, not too little. Get it just right, Goldilocks style.
4. Go Digital: Tech is your friend. Electronic records help avoid those oops moments in prescribing.
5. Team Huddle: Docs, nurses, and pharmacists all in the game. Best practices for hospital medication prescribing = teamwork.
6. Stay Updated: Keep up with the latest drug news and trends. You don’t wanna be that guy using outdated info.
Read Now : Patient-centered Medication Compliance Strategies
7. Listen Up: Patient’s feedback is gold. It’s part of best practices for hospital medication prescribing, you know?
8. Watch for Side Effects: Notice when things go south so you can tweak the plan.
9. Record Everything: If it ain’t written down, it didn’t happen. Best practices for hospital medication prescribing includes solid record-keeping.
10. Chill and Double-check: Mistakes happen when you’re rushing. Best practices for hospital medication prescribing means taking the time to do it right.
Multidisciplinary Approach in Medication Management
The collaborative effort among healthcare professionals is a pivotal aspect of implementing best practices for hospital medication prescribing. Engaging a multidisciplinary team ensures that the complexities of patient care are meticulously managed through shared expertise and a comprehensive understanding of pharmacotherapy. Physicians bring diagnostic precision and a deep comprehension of the patient’s medical history, while pharmacists offer extensive drug knowledge, ensuring that medication regimens are both safe and effective. Nurses play a crucial role in monitoring patient responses to medications, providing feedback that informs necessary adjustments and interventions.
This integrated approach exemplifies best practices for hospital medication prescribing by creating a dynamic environment where communication and cooperation mitigate the risk of errors. Regular interdisciplinary meetings and case discussions serve as platforms to evaluate treatment plans, allowing team members to contribute their insights and recommendations. Such collaboration fosters an environment of continuous learning and improvement, essential for maintaining the highest standards of patient care. By adhering to this model, healthcare institutions can ensure that their medication prescribing practices are robust, reliable, and patient-centric.
Moreover, the adaptation of technology within this framework further amplifies the efficacy of best practices for hospital medication prescribing. Electronic health records and communication tools streamline the sharing of crucial information, ensuring all team members have access to current and accurate data. This seamless information exchange supports swift decision-making and enhances the coordination of care. Ultimately, a multidisciplinary approach not only solidifies the foundation of best practices for hospital medication prescribing but also elevates the quality and safety of healthcare delivery.
Strategies for Enhancing Prescribing Practices
A strategic approach to enhancing hospital medication prescribing practices begins with fostering a culture of safety and accountability. Educating healthcare professionals about the critical importance of best practices for hospital medication prescribing is paramount. Regular training sessions and workshops can ensure that all staff are equipped with the necessary skills and knowledge to navigate complex prescribing decisions effectively. Moreover, establishing clear policies and guidelines that adhere to national and international standards reinforces consistency and reliability across the board.
Instituting robust error-reporting mechanisms also contributes to the refinement of prescribing practices. Encouraging open communication about errors without fear of retribution allows for the identification of systemic issues and the implementation of corrective measures. Additionally, leveraging data analytics to track and analyze prescribing trends enables healthcare institutions to identify areas for improvement and develop targeted interventions. By prioritizing a proactive approach, hospitals can anticipate potential issues and adapt their practices accordingly.
Finally, involving patients in the decision-making process is a vital component of best practices for hospital medication prescribing. Educating patients about their treatment plans and encouraging their active participation ensures a more tailored and effective approach to medication management. This patient-centered focus not only enhances adherence but also fosters a sense of empowerment and trust in the healthcare process. Through these comprehensive strategies, healthcare institutions can significantly elevate their prescribing practices, ensuring optimal outcomes for all patients.
Summary of Prescribing Best Practices
In summary, the implementation of best practices for hospital medication prescribing is crucial for optimizing patient care and enhancing healthcare outcomes. These practices hinge upon a thorough understanding of the patient’s medical history, vigilant awareness of potential drug interactions, and the precise tailoring of dosages to individual needs. The integration of electronic prescribing systems has become invaluable, reducing the likelihood of errors and streamlining the prescribing process. Moreover, the continuous education of healthcare professionals and the fostering of a collaborative environment involving multidisciplinary teams are essential components in maintaining high standards of care.
Furthermore, embracing a proactive approach through the use of data analytics and patient engagement is vital. Tracking prescribing patterns and encouraging patient feedback allows for the continuous refinement of practices, ensuring they are aligned with the latest evidence-based research. This comprehensive approach not only mitigates risks but also promotes a culture of safety and accountability within healthcare institutions. Ultimately, by steadfastly adhering to best practices for hospital medication prescribing, healthcare providers can deliver safe, effective, and patient-centric care that meets the highest standards of healthcare excellence.