The complexity of cancer treatment necessitates innovative approaches that can dynamically adjust to patient needs and disease progression. Adaptive treatment strategies in oncology have emerged as a promising paradigm, integrating real-time data and patient responses to personalize treatment plans effectively. These strategies can significantly improve treatment outcomes by responding to the changes in disease behavior and resistance profiles, thereby offering a flexible path in the management of cancer.
Read Now : Organic Skincare Routine Tips
Understanding Adaptive Treatment Strategies
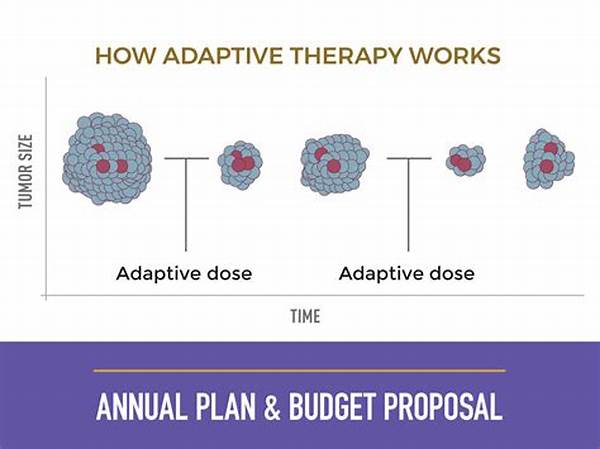
Adaptive treatment strategies in oncology refer to a methodological framework designed to tailor therapeutic interventions based on continuous patient monitoring and feedback. These strategies leverage advanced technologies, such as biomarkers and imaging, to adapt and optimize treatment regimens continually. The objective is to achieve a higher degree of personalization by adjusting therapeutic components, including dosage and drug combinations, in response to the evolving condition of the patient. This approach contrasts with traditional static treatment paradigms that often display less flexibility in accommodating the dynamic nature of cancer. The adaptability inherent in these strategies enables oncologists to proactively modify treatment plans to address issues such as drug resistance and adverse effects, ultimately improving clinical outcomes and quality of life for patients.
Core Principles of Adaptive Strategies
1. Personalization: Adaptive treatment strategies in oncology rely on individualized care, adjusting treatments based on genetic, physiological, and environmental factors.
2. Real-Time Monitoring: Integration of real-time data through regular assessments allows continuous adaptation of treatment modalities.
3. Dynamic Adjustments: These strategies involve ongoing modifications to therapeutic plans to counteract drug resistance and tumor adaptation.
4. Interdisciplinary Approach: Collaboration between oncologists, data scientists, and other specialists is essential to implement adaptive frameworks effectively.
5. Enhanced Patient Outcomes: The primary goal of adaptive treatment strategies in oncology is to increase the efficacy of cancer treatments, minimize adverse effects, and improve overall patient survival rates.
Technological Implications in Adaptive Strategies
The implementation of adaptive treatment strategies in oncology is revolutionizing the therapeutic landscape through technological advancements. Innovations in genetic sequencing, bioinformatics, and artificial intelligence play pivotal roles in facilitating adaptive methodologies. Genetic sequencing provides critical insights into tumor heterogeneity, enabling personalized adjustments to treatment protocols. Bioinformatics tools are utilized for the analysis and interpretation of large datasets, providing actionable insights for modifying treatment approaches. Furthermore, artificial intelligence and machine learning algorithms are instrumental in predicting patient responses, optimizing dosage regimens, and identifying novel therapeutic targets. Together, these technological components enhance the precision and efficiency of adaptive treatment strategies, ushering in a new era of oncological care where freedom and flexibility in treatment can drastically improve patient outcomes.
Slang Description of Adaptive Strategies
Adaptive treatment strategies in oncology are like having a tailor-made suit for each patient in the fight against cancer. They’re not static, they keep evolving, like a playlist that changes with every listen. Here are 10 quick takes:
1. Bespoke Plans: Every patient gets a unique treatment playbook.
2. Real-Time Tweaks: It’s like getting instant feedback and changing course as needed.
Read Now : Biomarkers Identification Through Genomics
3. Dynamic Duo: More like a conversation with your treatment, not a lecture.
4. Team Effort: Think of it as a jam session with experts from all fields.
5. Win-Win: The main gig is to better outcomes, less side hustle from side effects.
Personalized Medicine Paradigms
In the realm of personalized medicine, adaptive treatment strategies in oncology stand as a key pillar. Personalized medicine focuses on customizing healthcare, with decisions tailored to individual patients based on their predicted response or risk of disease. The adaptive strategies within oncology are particularly aligned with this vision, providing a framework that is patient-centered and responsive to the unique progression of their disease. By incorporating genetic, environmental, and lifestyle factors, these strategies strive to maximize therapeutic efficacy and minimize potential harm.
The success of adaptive treatment strategies in oncology as part of personalized medicine initiatives is heavily reliant on the integration of cutting-edge technologies and multidisciplinary collaboration. The rapid advancements in genomic technologies, particularly next-generation sequencing, allow for the comprehensive analysis of patient-specific tumor characteristics. This information is crucial for designing adaptive regimens that evolve with the patient’s disease, thereby increasing the chances of treatment success. Additionally, by leveraging data analytics and machine learning, adaptive strategies can offer dynamic insights, enabling timely decisions that improve patient outcomes.
Collaborative Frameworks for Adaptive Treatments
The implementation of adaptive treatment strategies in oncology necessitates a collaborative framework that draws on diverse expertise. At the heart of this framework is the interdisciplinary collaboration between oncologists, geneticists, data scientists, and other healthcare professionals. Such collaboration is crucial for integrating the advanced technologies and analytic techniques that are integral to adaptive strategies. Each discipline contributes unique insights and capabilities that enable the effective design, monitoring, and adjustment of treatment plans, ensuring they are as responsive and personalized as possible.
In addition to medical expertise, the role of the patient is central in adaptive treatment strategies in oncology. Patients are active participants in their care, and their feedback is vital to the adaptive process. Engagement with patients ensures that their experiences, preferences, and values are considered in the development of their treatment plans. Effective communication between patients and healthcare providers fosters a shared decision-making process, enabling treatments to be tailored to an individual’s needs and goals. This collaborative model enhances the potential of adaptive strategies to deliver personalized and effective cancer care.
Conclusion
In summary, adaptive treatment strategies in oncology represent a significant evolution in the approach to cancer treatment. These strategies embody a dynamic, patient-centered methodology that continuously refines treatment plans based on real-time patient data and disease progression. Emerging technologies, interdisciplinary collaboration, and a focus on individualized care are cornerstones of this approach, facilitating the delivery of more effective and personalized healthcare solutions. As these strategies continue to evolve, they hold great promise for improving outcomes in oncology, offering hope for a future where cancer treatment is as adaptive and unique as the patients themselves.