Antibiotics play a crucial role in treating bacterial infections. These medications work by eliminating or inhibiting the growth of harmful bacteria. To achieve optimal results, it is imperative that patients adhere to the prescribed course of treatment. Failing to do so can lead to unintended and often severe consequences. The consequences of not completing antibiotics are not only detrimental to individual health but can also pose significant public health risks.
Read Now : Nonverbal Communication In Medical Settings
Understanding the Significance of Antibiotic Completion
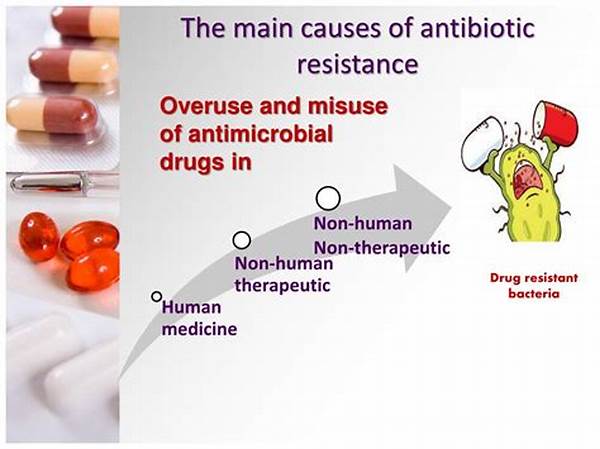
The primary consequence of not completing antibiotics is the potential for the infection to persist. When antibiotics are taken partially, some bacteria might survive, allowing the infection to linger or even worsen. This can necessitate additional treatment, increasing the risk of complications. Furthermore, incomplete antibiotic courses contribute to the development of antibiotic-resistant strains of bacteria. These bacteria become more challenging to treat and require more potent and potentially more toxic medications, complicating healthcare management. The broader public health implications include increased transmission of resistant bacteria, posing a threat to community health. Therefore, understanding the far-reaching consequences of not completing antibiotics emphasizes the importance of adhering to prescribed regimens.
Moreover, the consequences of not completing antibiotics extend to increased healthcare costs. Patients who do not finish their antibiotics as prescribed may require more intensive treatments, longer hospitalizations, or additional medications. This not only strains healthcare systems but also places a financial burden on patients and society. In summary, the individual and societal repercussions of neglecting the full course of antibiotics underscore the critical need for patient education and adherence to antibiotic prescriptions.
Key Consequences of Non-Adherence to Antibiotic Regimens
1. Persistent Infections: Incomplete antibiotic courses can result in persistent infections, requiring further medical intervention.
2. Development of Resistant Bacteria: Failure to complete antibiotics fosters antibiotic resistance, complicating future treatments.
3. Enhanced Health Risks: Patients face increased risks of complications and severe health outcomes when treatments are not completed.
4. Public Health Threat: Non-compliance contributes to the spread of resistant bacteria, posing widespread community health challenges.
5. Increased Healthcare Costs: Non-adherence can lead to more extensive and costly medical treatments, escalating financial strains.
The Public Health Implications of Incomplete Antibiotic Courses
The consequences of not completing antibiotics extend beyond the individual, posing considerable challenges to public health systems. Antibiotic resistance, exacerbated by incomplete courses, has become one of the most urgent health threats today. As resistant bacteria proliferate, infections become more difficult to treat, leading to longer hospital stays, higher medical costs, and increased mortality. Public health initiatives must focus on educating the community about the importance of completing antibiotic prescriptions. Encouraging adherence through awareness campaigns and healthcare provider interventions is pivotal in combating this growing threat. By understanding and addressing the public health implications, a concerted effort can be made to mitigate the consequences of not completing antibiotics.
In addition, incomplete antibiotic treatment can diminish the efficacy of future treatments for individuals and communities. As incidences of resistance grow, previously effective antibiotics may no longer yield the desired curative effects. This scenario increases the dependency on newer, potentially costlier, and more hazardous treatments. A global approach, involving collaboration between healthcare providers, policymakers, and patients, is essential to address the ramifications of incomplete antibiotic courses and to ensure effective management of bacterial infections.
Slang Perspective on Incomplete Antibiotics
1. It’s a bad move to ditch antibiotics mid-course; that’s how you get superbugs.
2. Stopping early? Say hello to stubborn germs!
3. You snooze, you lose—finish your meds, or the bugs bounce back.
4. Cutting corners with antibiotics can cost big time health-wise.
Read Now : Stem Cell Therapy Applications
5. Play the long game—finish that pill pack and avoid nasty surprises.
6. Don’t half-ass it, or you’re in for a rough ride with infections.
7. Finish your script, or you might need the big guns next time.
8. Going rogue on meds? Those germs just might level up.
9. Skipping meds is like leaving your team midway—don’t bail.
10. Break up with bacteria properly—strike out with meds all the way.
Importance of Education in Antibiotic Adherence
Engaging Healthcare Professionals
Enhancing patient education about antibiotics involves a collaborative healthcare team effort. Healthcare providers, including doctors, nurses, and pharmacists, play a key role in educating patients about the significance of completing antibiotic courses. By offering detailed explanations in simple language and addressing patient concerns, providers can foster a better understanding of antibiotic regimens and their importance. The consequences of not completing antibiotics should be clearly communicated, emphasizing not only individual health risks but also wider public health challenges.
Utilizing Technology for Better Communication
Leveraging technology can significantly improve patient adherence to antibiotic prescriptions. Digital platforms, such as mobile apps and online patient portals, can provide timely reminders, educational resources, and easy access to healthcare professionals for questions and concerns. These tools empower patients by keeping them informed and engaged with their treatment plans. By integrating technology with traditional healthcare practices, the gap between prescription and patient compliance can be effectively reduced.
Summary and Call to Action
In conclusion, the consequences of not completing antibiotics are multi-faceted, impacting both individual health and public well-being. Antibiotic resistance remains a growing concern, exacerbated by incomplete antibiotic courses. To address this issue, a concerted effort is required from all stakeholders, including healthcare providers, patients, and policymakers. Education plays a crucial role in ensuring patients understand the importance of completing their prescribed antibiotics.
Thus, it is imperative to implement robust education and awareness campaigns highlighting the dangers of antibiotic non-compliance. Healthcare institutions should actively engage patients through clear communication and accessible resources. Policymakers must support initiatives that encourage completion of antibiotic regimens, aiming for a significant reduction in antibiotic resistance. Tackling the consequences of not completing antibiotics requires a comprehensive approach, with a strong focus on patient education and adherence to prescribed treatments.