Understanding Evidence-Based Medical Practice Guidelines
In the realm of contemporary healthcare, evidence-based medical practice guidelines stand as pivotal components in the delivery of high-quality medical care. These guidelines are systematically developed statements designed to assist practitioners and patients in making informed decisions about appropriate healthcare for specific clinical circumstances. Rooted in a meticulous analysis of current research and clinical expertise, evidence-based medical practice guidelines aim to standardize care, minimize variations in practice, and ensure optimal patient outcomes.
Read Now : Patient-centered Healthcare Application Infrastructure
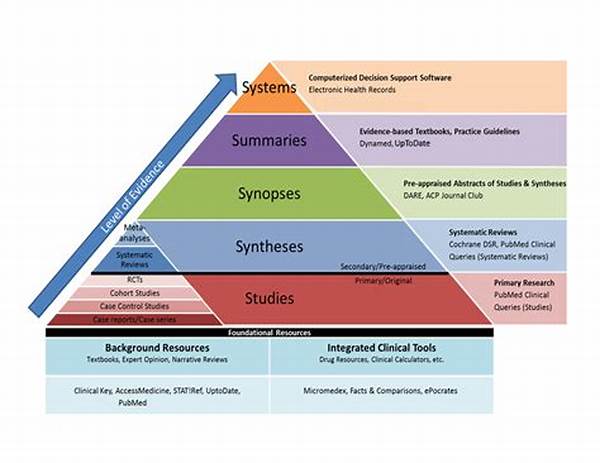
Such guidelines are formulated through the rigorous appraisal of evidence gathered from a multitude of sources. Systematic reviews, clinical trials, and expert opinions are synthesized to provide comprehensive recommendations for clinical practice. The objective is to bridge the gap between research and practice, translating scientific discoveries into practical interventions that enhance the quality of patient care. Evidence-based medical practice guidelines serve as a cornerstone in this endeavor, promoting consistent and effective treatment approaches across diverse healthcare settings.
Moreover, evidence-based medical practice guidelines play a crucial role in elevating the overall standard of care by fostering continuous professional development and education. Healthcare providers are encouraged to stay abreast of the latest guidelines to ensure that their clinical practices are aligned with current evidence. This commitment to continuous learning not only enhances the competence of practitioners but also inspires confidence among patients who seek assurance that their care is based on the most reliable and up-to-date information available.
The Importance of Adherence to Guidelines
1. Evidence-based medical practice guidelines represent a synthesis of research and clinical expertise, providing healthcare providers with robust frameworks for delivering patient care. Adherence to these guidelines ensures that treatment decisions are made based on credible evidence, thereby optimizing patient outcomes and reducing the risk of adverse events.
2. The implementation of evidence-based medical practice guidelines encourages uniformity in healthcare delivery, minimizing unwarranted variations in treatment approaches. This standardization is essential in maintaining the integrity of health services, ensuring that all patients receive care that is consistent with the highest standards of medical knowledge.
3. Evidence-based medical practice guidelines facilitate the integration of new research findings into clinical practice, ensuring that healthcare providers have access to the most current and relevant information. This dynamic process promotes the advancement of medical science while directly benefiting patient care through informed clinical decisions.
4. Adherence to evidence-based medical practice guidelines enhances accountability among healthcare practitioners by providing a clear framework for evaluating clinical practice. This accountability is crucial for maintaining trust between patients and providers, fostering transparency, and upholding the ethical standards of the medical profession.
5. The use of evidence-based medical practice guidelines supports informed patient engagement, enabling individuals to participate actively in their healthcare decisions. By understanding the basis of recommended treatments, patients are empowered to make choices that align with their values and preferences, ultimately leading to improved satisfaction and health outcomes.
Developing Robust Evidence-Based Guidelines
The development of evidence-based medical practice guidelines involves a comprehensive and meticulous process aimed at ensuring their reliability and relevance. Central to this process is the systematic identification and appraisal of available evidence, which underpins the recommendations contained within these guidelines. The involvement of multidisciplinary experts, including clinicians, researchers, and statisticians, is vital in ensuring that the guidelines are both clinically applicable and scientifically rigorous.
An essential step in developing evidence-based medical practice guidelines is the critical appraisal of literature, where evidence is evaluated for its quality, consistency, and applicability. This appraisal is guided by predefined criteria that prioritize the inclusion of high-quality studies, such as randomized controlled trials and systematic reviews. The inclusion of diverse expert opinions further enriches the guideline development process, ensuring that diverse perspectives are considered and that the recommendations are feasible for implementation in varied clinical settings.
Finally, evidence-based medical practice guidelines undergo continuous evaluation and updating to remain aligned with the latest scientific discoveries and advancements in clinical practice. This iterative process of refinement ensures that the guidelines remain relevant and that practitioners are equipped with the most current evidence to support their clinical decision-making. In this way, evidence-based medical practice guidelines play a critical role in fostering the evolution of healthcare practices and improving patient outcomes.
Evidence-Based Guidelines in Everyday Language
Evidence-based medical practice guidelines, often referred to as the “gold standard” in healthcare, are basically rulebooks that doctors follow to make sure they’re giving top-notch care rooted in proven research. These guidelines keep everyone on the same page, so no matter where you are, the medical advice is consistent and trustworthy.
1. These guidelines cut through the noise and hype, making it clear what’s genuinely beneficial and what’s just trendy. Doctors rely on these to avoid fads that might not be effective.
2. Think of these guidelines like a recipe for baking a cake; they ensure every doctor knows the right ingredients (or treatments) to use, aiming for the best outcome every time.
3. They’re like cheat sheets for doctors, reminding them of the latest and greatest in medical research, ensuring patient care is always top-tier.
4. Following these guidelines is like hitting a “reset” button; all patients get treated fairly with the most current medical advice.
5. Evidence-based guidelines are accountability tools, making sure healthcare providers are delivering the best care without cutting corners.
Read Now : Pharmaceutical And Herbal Safety Guidelines
6. They’re like a backup for second opinions; evidence-based medical practice guidelines legitimize the doctor’s advice with solid proof.
7. Doctors use these guidelines to stay hip with medical advancements, always learning and refining their practice based on real data.
8. They empower patients too, giving a sense of control, as patients understand why certain treatments are suggested.
9. It’s peace of mind knowing that healthcare isn’t just guesswork but is guided by something studied and verified.
10. Ultimately, these evidence-based guidelines aim for equal healthcare access and quality, regardless of where one resides.
The Role of Technology in Implementing Guidelines
Advancements in technology have revolutionized the manner in which evidence-based medical practice guidelines are developed, implemented, and accessed. Digital platforms and databases provide healthcare professionals with immediate access to a wealth of up-to-date guidelines, facilitating seamless integration into clinical practice. Tools such as electronic health records (EHRs) and clinical decision support systems (CDSS) further promote adherence to these guidelines by providing real-time alerts and recommendations pertaining to patient care.
Additionally, technology enables the systematic analysis of large datasets, which can be used to refine and improve existing guidelines. Big data analytics and artificial intelligence offer sophisticated mechanisms for uncovering patterns and insights that inform guideline development. This intersection of technology and medicine underscores the dynamic nature of evidence-based medical practice guidelines, emphasizing the importance of continual adaptation and refinement to accommodate emerging research findings.
Moreover, technology-driven platforms enable collaborative efforts among multidisciplinary teams working on guideline development. Communication tools and virtual workspaces facilitate the exchange of ideas and expertise, enhancing the comprehensiveness of guidelines and ensuring their relevance across diverse healthcare contexts. The integration of technology not only strengthens the formulation and dissemination of evidence-based medical practice guidelines but also serves as a catalyst for innovation in patient care.
Challenges in Adhering to Guidelines
Despite the acknowledged benefits, the implementation of evidence-based medical practice guidelines is not without challenges. Among the most notable obstacles is the resistance to change often encountered within the medical community. Providers accustomed to established practices may hesitate to adopt new guidelines, particularly if they perceive substantial deviation from their traditional approaches. This resistance can hinder the widespread acceptance and use of evidence-based medical practice guidelines.
Furthermore, the sheer volume and complexity of medical guidelines present a significant challenge. Practitioners may find it difficult to keep abreast of numerous updates across various specialties, potentially leading to inconsistent application of the most current evidence. This issue is compounded by limited time and resources, which can impede the in-depth study and implementation of comprehensive guidelines.
Finally, healthcare systems may face logistical and infrastructural barriers that impact the practical application of evidence-based medical practice guidelines. Variations in resource availability, staffing, and organizational support can contribute to differing levels of adherence to these guidelines. Addressing these challenges requires strategic efforts to promote education, foster collaboration, and enhance accessibility to updated guidelines across all levels of the healthcare system.
Summary of Evidence-Based Medical Practice Guidelines
In conclusion, evidence-based medical practice guidelines are indispensable tools in the pursuit of excellence in healthcare delivery. By providing a systematic framework for clinical decision-making, these guidelines ensure that patient care is grounded in the best available evidence. They bridge the gap between research and practice, empowering healthcare providers to deliver treatments that are both effective and efficient.
The benefits of adhering to evidence-based medical practice guidelines are manifold, encompassing improved patient outcomes, enhanced accountability, and the promotion of standardized care delivery. These guidelines facilitate ongoing learning and adaptation, encouraging practitioners to remain informed about advancements in medical science. Additionally, the integration of technology in the development and dissemination of guidelines amplifies their impact, ensuring they remain relevant and accessible in an ever-changing healthcare landscape.
Ultimately, the successful implementation of evidence-based medical practice guidelines hinges on the collective commitment of healthcare providers, researchers, and policymakers. By prioritizing continuous education, fostering interdisciplinary collaboration, and supporting systems that enable guideline adherence, stakeholders can work toward the realization of a healthcare system that is both responsive and accountable to the needs of patients. In this way, evidence-based medical practice guidelines remain a cornerstone of modern medicine, guiding the path toward improved health and well-being for all.