Introduction to Genetic Screening in Clinical Practice
Genetic screening in clinical practice represents a sophisticated and valuable tool for the early detection and management of genetic disorders. Its integration into healthcare settings has significantly transformed the landscape of diagnostic and preventive medicine. In recent years, advancements in genome sequencing technologies have further augmented the capabilities and accuracy of genetic screening, allowing clinicians and researchers to gain a more comprehensive understanding of an individual’s genetic makeup. This has paved the way for personalized medicine, wherein healthcare providers can tailor interventions and treatments to the unique genetic profile of each patient. The implications of genetic screening are vast, spanning from prenatal diagnosis to adult-onset conditions, thus making it an indispensable component of modern clinical practice.
Read Now : Holistic Approach To Well-being
Incorporating genetic screening into routine medical assessments enables healthcare professionals to identify individuals at risk of inheriting or developing genetic disorders. Early identification and intervention can lead to improved management strategies and potentially mitigate the impact of these conditions. This proactive approach not only benefits individuals but also holds promise for reducing the overall burden on healthcare systems by addressing potential health issues before they manifest. Furthermore, genetic screening in clinical practice is invaluable for guiding reproductive decision-making, offering prospective parents critical insights into their genetic predispositions and the likelihood of passing hereditary conditions to their offspring.
Despite its considerable advantages, genetic screening in clinical practice raises ethical, legal, and social considerations. Ensuring patient confidentiality, informed consent, and the responsible handling of genetic information are paramount for maintaining public trust and safeguarding individuals’ rights. As genetic technologies continue to evolve, healthcare providers must navigate these challenges while harnessing the potential benefits that genetic screening offers. In this dynamic and rapidly advancing field, ongoing research and collaboration among clinicians, geneticists, ethicists, and policymakers are essential to optimize the integration of genetic screening into clinical practice and realize its full potential in enhancing patient care.
The Benefits of Genetic Screening in Clinical Practice
1. Genetic screening in clinical practice facilitates early detection of genetic disorders, allowing for timely medical interventions and minimizing disease progression.
2. It provides insights for personalized medicine by tailoring treatments and therapies based on an individual’s unique genetic makeup, enhancing treatment efficacy.
3. Genetic screening in clinical practice aids in identifying carriers of genetic conditions, informing reproductive choices, and reducing the transmission of hereditary diseases.
4. It contributes to better health outcomes by enabling preventive measures, lifestyle modifications, and informed decision-making for individuals at risk.
5. Genetic screening in clinical practice supports research and data collection, advancing our understanding of genetic disorders and ultimately improving future clinical practices.
Ethical Considerations in Genetic Screening in Clinical Practice
The integration of genetic screening in clinical practice raises significant ethical considerations that necessitate careful examination and deliberation. One of the foremost concerns is ensuring the confidentiality and protection of individuals’ genetic information. The sensitive nature of genetic data necessitates stringent safeguards to prevent unauthorized access, misuse, or discrimination. Addressing issues of privacy and data security is paramount to maintain public trust in genetic screening practices and protect individuals from potential harm or prejudice.
Informed consent is another critical aspect of genetic screening in clinical practice. Patients must be fully informed about the purpose, benefits, risks, and limitations of genetic screening before making decisions about their participation. This requires transparent communication between healthcare providers and patients to ensure that individuals understand the implications of genetic screening results and can make autonomous decisions. Moreover, healthcare providers must address potential psychological impacts, such as anxiety or distress, that may arise from the knowledge of genetic predispositions to certain conditions. By navigating these ethical considerations thoughtfully, the medical community can foster responsible and equitable utilization of genetic screening in clinical practice, thus enhancing patient autonomy and care.
Challenges and Limitations of Genetic Screening in Clinical Practice
Despite its transformative potential, genetic screening in clinical practice is not without challenges and limitations. The rapid progression of genetic technologies outpaces the development of comprehensive guidelines and standardized practices, leading to variability in the implementation and interpretation of screening results. Additionally, not all genetic conditions have known treatments or interventions, which can result in uncertainty and ethical dilemmas for both patients and healthcare providers. As such, ongoing research and rigorous clinical validation are paramount to ensure the reliability and clinical utility of genetic screening.
Healthcare professionals must also consider the implications of incidental findings, where unexpected genetic results unrelated to the primary reason for testing may arise. The management of such findings calls for clear protocols and guidelines to address the potential emotional and medical impacts on patients. Another challenge lies in ensuring equitable access to genetic screening, as socioeconomic disparities can limit individuals’ ability to benefit from these advancements. Genetic screening in clinical practice requires a commitment to continuous education, ethical considerations, and the development of policies that promote fair access and responsible use of genetic information.
Genetic Screening in Clinical Practice: A Casual Perspective
1. Genetic screening in clinical practice is like having a crystal ball for your health. It gives you a sneak peek into what might be down the road, health-wise.
2. Think of it as a DNA blueprint. With genetic screening in clinical practice, doctors can create a personalized health game plan just for you.
3. Ever wanted a heads-up on health risks? Genetic screening in clinical practice does just that, helping people dodge potential health curveballs.
4. For future parents, genetic screening in clinical practice is a real game-changer. It lets you in on what to expect in terms of passing on genetic traits.
Read Now : Moral Implications Of Regenerative Medicine
5. Not all about the genes? No worries, genetic screening in clinical practice shows how lifestyle and environment mix with your DNA to shape your health.
6. While it’s super helpful, genetic screening in clinical practice can raise eyebrows. People might stress over what their genes reveal.
7. Health choices made easy with genetic screening in clinical practice — big decisions feel a lot lighter with solid info at your side.
8. It’s essential to handle your results with care. With genetic screening in clinical practice, knowing how to interpret findings can be tricky.
9. Accessibility is a thing: genetic screening in clinical practice isn’t always within arm’s reach for everyone, which can be a bummer.
10. At the end of the day, genetic screening in clinical practice offers a peek into possible future health scenarios, making it a powerful ally in the medical world.
Implementing Genetic Screening in Clinical Practice
Implementing genetic screening in clinical practice necessitates a multidisciplinary approach that involves collaboration among geneticists, clinicians, and healthcare administrators. The successful integration of genetic screening within healthcare systems relies on developing standardized procedures and frameworks to ensure consistency and accuracy. Training healthcare professionals in genetic literacy and counseling is crucial to effectively communicate results and their implications to patients. By establishing clear protocols, healthcare providers can navigate the complexities of genetic screening while maintaining patient-centric care.
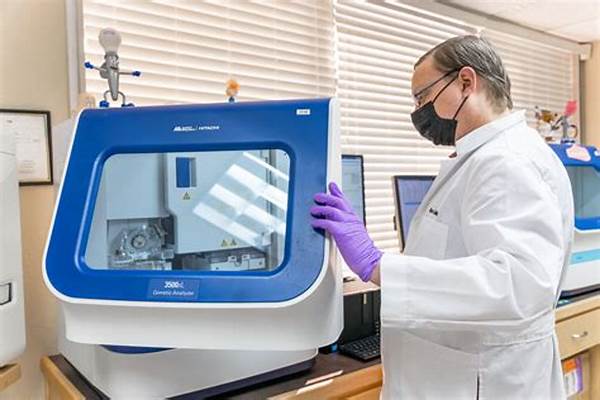
Moreover, implementing genetic screening in clinical practice requires adequate infrastructure to handle sensitive genetic information securely. Investment in advanced laboratory technologies and data management systems is essential to facilitate the accurate analysis and storage of genetic data. Furthermore, ensuring equitable access to genetic screening remains a priority to prevent disparities and guarantee that all individuals can benefit from these advancements. As genetic screening continues to grow, it is vital for healthcare institutions to remain agile, adapting to emerging technologies and evidence to optimize patient care.
Transforming Patient Care through Genetic Screening in Clinical Practice
The advent of genetic screening in clinical practice has revolutionized patient care by offering tailored healthcare solutions based on genetic insights. Personalized medicines, guided by genetic data, allow clinicians to develop treatment plans that are more effective and precise, minimizing adverse reactions and optimizing therapeutic outcomes. Genetic screening enables early identification of individuals at risk for specific conditions, contributing to preventive measures and improved management strategies.
Furthermore, genetic screening in clinical practice empowers patients by providing them with comprehensive knowledge about their genetic predispositions and health risks. Armed with this information, patients can make more informed decisions regarding lifestyle modifications, reproductive choices, and healthcare interventions. The synergy of advanced genetic technologies and personalized patient care holds immense potential for advancing clinical practice and ultimately improving health outcomes on an individual and population level.
Conclusion: The Future of Genetic Screening in Clinical Practice
In conclusion, genetic screening in clinical practice represents a paradigm shift in healthcare, offering unprecedented opportunities for early diagnosis, targeted interventions, and personalized treatment strategies. As technology advances, the potential applications of genetic screening will continue to expand, shaping the future of healthcare. However, challenges such as ethical considerations, data security, and equitable access must be addressed to maximize the benefits while mitigating potential risks.
The integration of genetic screening in clinical practice necessitates a commitment to interdisciplinary collaboration, ongoing research, and policy development to ensure responsible and effective utilization. Embracing these advancements has the potential to not only improve individual patient outcomes but also transform the broader healthcare landscape, enhancing the quality and efficiency of care provided. As the field evolves, it is essential for healthcare professionals, researchers, and policymakers to work collaboratively to realize the full potential of genetic screening in clinical practice.