Pharmacokinetic analysis in clinical dosing plays a pivotal role in the realm of personalized medicine, marking a significant advancement in healthcare. By examining how drugs are absorbed, distributed, metabolized, and excreted in the human body, pharmacokinetic analysis ensures a precise and tailored approach to medication management. This scientific discipline addresses the variability in drug response among individuals, a factor significantly influenced by genetic, physiological, and environmental variables. The core aim of pharmacokinetic analysis in clinical dosing is to optimize therapeutic efficacy while minimizing toxicity. By implementing pharmacokinetic principles, clinicians are equipped to calculate the appropriate drug dosage and frequency for each patient, thereby enhancing treatment outcomes. Consequently, this approach not only improves patient safety but also enhances the overall quality of care.
Read Now : Person-centered Communication Methodologies
The Role of Pharmacokinetics in Dosage Calculation
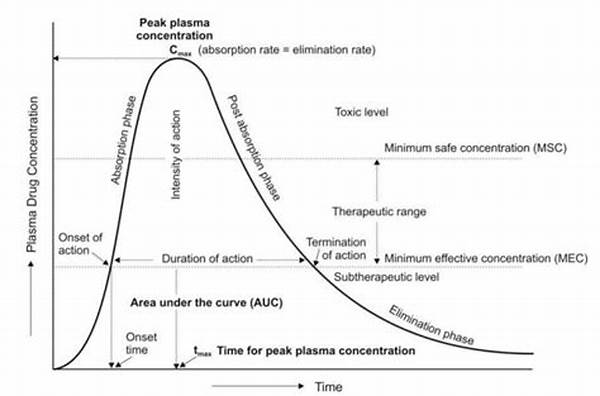
Pharmacokinetic analysis in clinical dosing is essential for determining the precise dosage of medications. It encompasses various parameters such as absorption rate, bioavailability, and clearance, facilitating accurate dosage calculations to achieve the desired therapeutic outcomes. This understanding helps healthcare professionals tailor treatments to individual patient needs, ensuring both efficacy and safety.
Pharmacokinetic analysis in clinical dosing serves as an indispensable tool in treatment personalization. By studying drug behavior, clinicians can make informed decisions regarding dosage adjustments. This process accounts for individual patient characteristics, promoting effective therapeutic interventions while mitigating adverse reactions and enhancing patient compliance.
Pharmacokinetic analysis in clinical dosing allows for an in-depth examination of drug interactions. Comprehending these interactions helps in identifying potential risks and optimizing therapeutic regimens. By evaluating how different drugs impact each other’s pharmacokinetics, healthcare providers can avoid harmful effects, ensuring patient safety and maximizing therapeutic potential.
Through pharmacokinetic analysis in clinical dosing, clinicians can forecast the half-life of drugs, aiding in determining optimal dosing intervals. By understanding the half-life, medical professionals can prevent drug accumulation and toxicity. This information is critical for chronic treatments, where maintaining steady blood levels is paramount for efficacy.
The integration of pharmacokinetic analysis in clinical dosing with pharmacogenomics further enhances personalized medicine. By understanding genetic variations in drug metabolism and response, healthcare providers can refine dosing regimens to match individual genetic profiles. This synergy between pharmacokinetics and genetics optimizes efficacy, reduces adverse effects, and revolutionizes patient care.
Clinical Applications of Pharmacokinetic Analysis
Pharmacokinetic analysis in clinical dosing has a wide range of applications in modern healthcare. One prominent application is in the realm of chronic disease management, where consistent and precise dosing is critical. For instance, in the management of conditions like epilepsy or hypertension, where long-term therapy with specific medication levels is required, pharmacokinetic principles guide clinicians in establishing a therapeutic regimen that maintains drug concentrations within the therapeutic window. This reduces the risk of sub-therapeutic dosing or toxicity, thus ensuring sustained disease control.
Additionally, pharmacokinetic analysis in clinical dosing is instrumental in adjusting therapies according to patient-specific factors. In special populations, such as pediatric or geriatric patients, pharmacokinetic parameters like absorption rates, body mass, and organ function can vary significantly. By incorporating these variables into drug dosing calculations, healthcare providers can customize treatment plans that are both safe and effective. This individualized approach transforms standard treatment protocols into tailored therapeutic strategies, thereby optimizing patient outcomes across diverse patient demographics.
Comprehensive Understanding Through Pharmacokinetic Studies
Understanding pharmacokinetic analysis in clinical dosing involves grasping the complex interactions between physiological processes and drug dynamics. This analysis provides insights into how drugs behave at different stages of their journey through the body, from the initial administration to eventual elimination. Pharmacokinetic studies elucidate the impact of biological factors such as age, weight, liver and kidney function, and co-morbid conditions on drug metabolism and clearance. Such comprehensive knowledge is critical for healthcare providers to tailor medical treatments accurately and predict patient-specific drug responses.
The pharmaceutical industry and regulatory bodies leverage pharmacokinetic analysis to design safer and more effective drugs. During drug development, pharmacokinetic profiling helps identify optimal dosing regimens and potential interactions with other medications. This understanding is crucial in defining testable hypotheses for clinical trials and mitigating risks associated with adverse drug reactions. By focusing on pharmacokinetic parameters, pharmaceutical companies can improve drug labels and provide detailed instructions for use, ultimately contributing to enhanced patient safety and therapeutic success. Thus, pharmacokinetic analysis in clinical dosing remains an integral component of both drug development and individualized patient care strategies.
Demystifying Pharmacokinetic Analysis with Slang Terms
So, you’re diving into pharmacokinetic analysis in clinical dosing. It’s basically checking out how drugs vibe in your body—where they travel, groove, and finally crash (get out). By knowing this stuff, docs can tailor your med party, ensuring you’re chill without any unwanted buzz.
1. Drug Vibe: It’s all about how meds travel and party in your body.
2. The Groove: Key to spotting how drugs work at different levels.
3. Crash Point: Understanding where drugs exit, so no overstay.
Read Now : Stress Reduction With Qi Gong
4. Custom Med Party: Tailored dosing ensuring you stay tuned.
5. Chill Mode: Maintaining steady drug levels for optimal chill.
6. Buzz Control: Avoiding unwanted reactions with precise dosing.
7. Groove Analysis: Spotting the groove is key to personalized meds.
8. Party Tailoring: Custom fitting your med to suit your needs.
9. Vibe Science: Using data to tweak the drug’s path for you.
10. Constant Tune: Ensures the right track keeps playing in your system.
Complexities in Pharmacokinetic Calculations
Delving deeper into pharmacokinetic analysis in clinical dosing unveils intricate calculations that extend beyond basic dosage determination. These complexities encompass diverse pharmacokinetic models which delineate drug kinetics for varying routes of administration. For instance, different models address intravenous and oral drug delivery, each requiring unique assumptions and methodologies for accurate predictions. Understanding these models necessitates proficiency in mathematical computations and a firm grasp of physiological processes, both crucial for precise dosage recommendations.
Advanced pharmacokinetic analyses also consider multi-compartmental models, which describe drug movement between various body compartments. This approach accounts for factors like tissue binding and delayed drug distribution, projecting a comprehensive understanding of drug events post-administration. These models are essential for drugs demonstrating non-linear kinetics, where changes in dose do not correspond linearly with blood concentration shifts. Thus, pharmacokinetic analysis in clinical dosing demands an integrative approach, balancing theoretical frameworks with empirical data to guide informed clinical decisions. This multidimensional strategy underpins the utility of pharmacokinetic insights in fostering safe and effective therapeutic practices across a myriad of clinical scenarios.
Integrating Pharmacokinetics with Clinical Practice
Integrating pharmacokinetic analysis in clinical dosing into everyday medical practice is a sophisticated endeavor requiring collaboration among clinicians, pharmacists, and researchers. This amalgamation aims to streamline patient management by utilizing pharmacokinetic data to inform drug prescription practices. Within clinical settings, physicians rely on pharmacokinetic principles to interpret laboratory data and patient-specific variables, thereby customizing treatment outlines. This approach enhances the efficacy of prescribed medicines while curtailing adverse drug reactions.
Moreover, the introduction of technology and software advancements has revolutionized pharmacokinetic analysis integration. These tools automate calculations and provide clinicians with comprehensive and accessible pharmacokinetic profiles for individual patients, enabling real-time data-driven decisions. The fusion of pharmacokinetic data with electronic health records further accelerates personalized dosing initiatives, fostering a data-rich environment for safe and informed therapeutic interventions. Consequently, the incorporation of pharmacokinetics into clinical practice not only maximizes treatment precision but also reinforces patient safety, leveraging scientific insights to elevate medical standards and healthcare quality.