In the realm of healthcare, understanding and managing prescription drug interactions is crucial for ensuring patient safety and efficacy of treatment. Drug interactions can result in diminished therapeutic effectiveness, increased toxicity, or unexpected side effects. Consequently, healthcare professionals and patients must remain vigilant in recognizing the potential consequences of these interactions and work collaboratively to mitigate risks.
Read Now : Tailoring Medical Treatments With Genetics
The Impact of Prescription Drug Interactions
Prescription drug interaction consequences can manifest in various forms, affecting multiple aspects of a patient’s health. One significant consequence is the alteration in the pharmacokinetics of a drug; interactions may change how a drug is absorbed, distributed, metabolized, or excreted, leading to suboptimal therapeutic levels or accumulation of drugs in the body. This alteration can either enhance a drug’s effect, resulting in toxicity, or reduce its effectiveness, failing to provide the intended therapeutic benefit.
Another critical consequence of prescription drug interactions is the potential for adverse drug reactions (ADRs). ADRs are unintended, harmful responses that can occur when drugs interact. These reactions can range from mild discomforts, such as nausea or headaches, to severe complications like organ failure or life-threatening anaphylaxis. Understanding these consequences underlines the importance of careful monitoring and adjustment of medication regimens.
Additionally, prescription drug interaction consequences place a significant burden on healthcare systems. Adverse interactions often lead to increased hospitalizations, extended healthcare costs, and additional medical interventions. By proactively addressing and preventing these interactions, healthcare providers can improve patient outcomes and reduce the economic impact on healthcare systems. Education and consistent communication between healthcare providers and patients are essential to managing these potentially serious consequences effectively.
Examples of Prescription Drug Interaction Consequences
1. Certain antibiotic prescriptions can reduce the efficacy of oral contraceptives, leading to unintended pregnancies, thus highlighting the importance of understanding prescription drug interaction consequences.
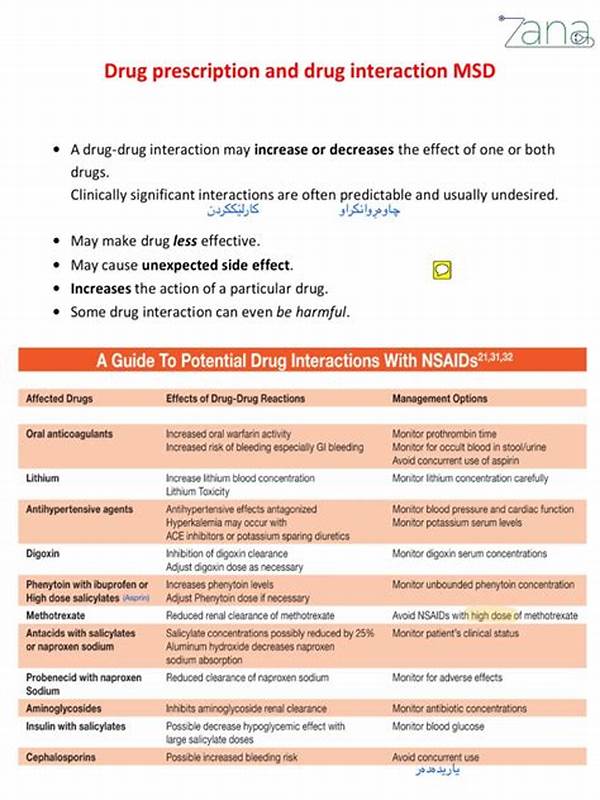
2. Concomitant use of anticoagulants and NSAIDs can increase bleeding risks due to prescription drug interaction consequences, necessitating careful monitoring by healthcare providers.
3. Antidepressants interacting with certain migraine medications can lead to serotonin syndrome, a severe condition resulting from prescription drug interaction consequences.
4. The combination of multiple antihypertensive agents can lead to dangerously low blood pressure, a significant prescription drug interaction consequence requiring dosage adjustments.
5. Prescription drug interaction consequences also include potential negative impacts on glucose levels when antidiabetic drugs are combined with other medications, requiring diligent monitoring of blood sugar.
Navigating Prescription Drug Interaction Risks
The healthcare sector must proactively address the risks associated with prescription drug interactions to minimize negative outcomes. Prescription drug interaction consequences can be mitigated through comprehensive medication reviews conducted by pharmacists and physicians, who can assess potential interactions and make necessary adjustments to treatment regimens. Employing electronic health records and drug interaction databases allows healthcare providers to access critical information, enabling more informed decision-making.
Patients play a crucial role in managing prescription drug interaction consequences as well. Being well-informed about their medications, actively communicating with healthcare providers, and adhering to prescribed regimens are essential steps that patients should embrace. Education initiatives aimed at enhancing patient awareness about the importance of prescription adherence and the risks posed by potential interactions can significantly reduce adverse outcomes.
Collaboration among healthcare professionals is essential to achieving optimal patient outcomes in managing prescription drug interaction consequences. Interdisciplinary teams can assess the risks associated with complex drug regimens, ensuring that all aspects of a patient’s health are considered. Through continuous education and research aimed at understanding drug interactions, healthcare systems can reduce the incidence of adverse effects and enhance patient safety.
Prescription Drug Interactions in Everyday Language
1. When meds don’t mix, it can get ugly fast. Prescription drug interaction consequences are no joke, causing side effects that mess with your life.
2. Take a chill pill, but not with grapefruit juice! Prescription drug interaction consequences can sneak up on you in unexpected ways.
3. Mixing meds can lead to drama. That’s why knowing prescription drug interaction consequences is key for staying healthy.
4. Watch out for combo chaos! Prescription drug interaction consequences mean some drugs shouldn’t party together in your system.
Read Now : Precision-based Herbal Remedies
5. Keeping tabs on your meds helps avoid those nasty prescription drug interaction consequences. It’s all about playing it smart!
6. Mixing meds like cocktails? Think again! Prescription drug interaction consequences can be a real buzzkill.
7. Getting hit with unexpected symptoms? It might be those prescription drug interaction consequences rearing their ugly head.
8. Sidestep the med mayhem by learning about prescription drug interaction consequences before they catch you off guard.
9. No one wants surprises when it comes to health. That’s why understanding prescription drug interaction consequences is clutch.
10. Keep your health in check by being aware of prescription drug interaction consequences. It’s the street-smart way to handle meds.
Understanding the Mechanisms of Interaction
Exploring the mechanisms that underpin prescription drug interaction consequences offers critical insights into their prevention and management. At the molecular level, these interactions often occur because drugs influence each other’s metabolism. Enzymatic pathways, particularly those involving cytochrome P450 enzymes, are frequently implicated. Certain medications can induce or inhibit these enzymes, leading to increased or reduced levels of concurrent drugs. By understanding these pathways, healthcare professionals can better predict and manage the outcomes of drug interactions, thereby reducing the incidence of adverse effects such as toxicity or therapeutic failure.
In addition to metabolic interactions, prescription drug interaction consequences can also result from pharmacodynamic interactions, where drugs influence each other’s effects at receptor sites or in physiological pathways. For instance, combining drugs with similar effects, such as central nervous system depressants, can result in excessive sedation or respiratory depression. Conversely, antagonistic interactions may reduce the efficacy of treatment, as seen with certain antihypertensive and non-steroidal anti-inflammatory drugs. A comprehensive understanding of these interactions helps clinicians devise strategies that ensure patient safety while maintaining therapeutic efficacy.
Strategies for Mitigating Prescription Drug Interaction Consequences
To effectively mitigate prescription drug interaction consequences, healthcare professionals must adopt a multifaceted approach. Comprehensive medication reconciliation is pivotal, particularly during care transitions, such as hospital admissions or discharges. This practice entails comparing a patient’s current medication regimen with new prescriptions to identify potential interactions. Additionally, employing clinical decision support systems integrated within electronic health records can provide real-time alerts to prescribers about possible interactions, thereby enhancing patient safety.
Education and communication form another cornerstone in minimizing prescription drug interaction consequences. Educating patients about the importance of disclosing all medications, including over-the-counter drugs and supplements, empowers them to participate actively in their healthcare. Meanwhile, fostering open channels of communication among healthcare providers ensures that all parties are informed about a patient’s medication history, facilitating coordinated care. These combined efforts are instrumental in identifying, avoiding, and managing potential prescription drug interaction consequences, ultimately enhancing patient outcomes and safety.
Summary of Prescription Drug Interaction Consequences
In conclusion, the consequences of prescription drug interactions present significant challenges to both patients and healthcare providers. These interactions can alter the intended therapeutic effects of medications, leading to adverse drug reactions that can range from mild to life-threatening. Furthermore, prescription drug interaction consequences extend beyond health implications, imposing financial burdens on healthcare systems through increased hospitalizations and treatments. Hence, effective strategies that incorporate comprehensive medication management, education, and communication are necessary to mitigate these risks proactively.
Healthcare professionals must remain vigilant in monitoring medication regimens and adjusting prescriptions as needed to address potential interactions. Interdisciplinary collaboration, coupled with the utilization of electronic tools, enhances the detection and prevention of adverse interactions. Meanwhile, patients’ active engagement in their treatment plans, guided by informed dialogue with their healthcare providers, can significantly reduce the incidence of negative prescription drug interaction consequences. In essence, a collective commitment to understanding and managing these interactions is paramount to ensuring safe and effective healthcare delivery.