The rapid advancement of both pharmaceutical and herbal industries has provided numerous options for health care. However, as the use of herbal supplements in conjunction with prescribed medications increases, understanding drug-herb interactions remains crucial. When these two elements are combined, interactions may occur that affect the efficacy and safety of the treatments involved. With the potential for unintended consequences, a deep understanding of drug-herb interactions is vital for both medical professionals and patients.
Read Now : Effective Work-life Balance Strategies
The Importance of Understanding Drug-Herb Interactions
As the line between traditional and modern medicine blurs, the importance of understanding drug-herb interactions cannot be overstated. Healthcare professionals must consider how herbs, such as St. John’s Wort, Ginkgo Biloba, or Echinacea, interact with common medications like anticoagulants or antidepressants. Such interactions can result in reduced drug efficacy, enhanced side effects, or even toxic effects, posing significant risks to patient health. Therefore, thorough research and awareness are indispensable in assessing the potential impact of these interactions.
In clinical settings, understanding drug-herb interactions is fundamental for ensuring optimal patient care. For patients who self-medicate with herbal supplements, the risk of unknown interactions increases. Physicians must inquire about herbal use when prescribing medications and consider the possibility of interactions when unexpected side effects arise. Empowering patients with information about potential interactions encourages informed decision-making, fostering a partnership between healthcare providers and patients.
Mechanisms of Drug-Herb Interactions
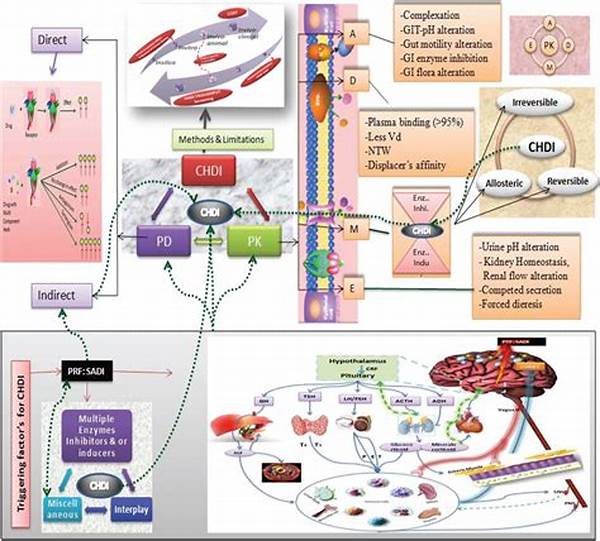
1. Pharmacodynamic Interactions: Understanding drug-herb interactions includes recognizing how herbs can alter pharmacodynamics by affecting drug-receptor interactions, potentially leading to increased side effects or diminished efficacy.
2. Pharmacokinetic Interactions: Important factors involve changes in the absorption, distribution, metabolism, and excretion of a drug due to herbal supplements, impacting overall drug levels and responses.
3. CYP450 Enzyme Modulation: Many herbs can induce or inhibit the cytochrome P450 enzymes, vital in drug metabolism, thus understanding drug-herb interactions helps foresee changes in drug clearance.
4. Synergistic Effects: Certain herbs might have synergistic effects with drugs, enhancing therapeutic outcomes or exacerbating toxicity, underscoring the importance of understanding drug-herb interactions.
5. Herbal Constituents’ Variability: The variability in the active constituents of herbs adds complexity to predicting interactions, reinforcing the need for comprehensive understanding of drug-herb interactions.
Challenges in Understanding Drug-Herb Interactions
In understanding drug-herb interactions, several challenges must be addressed, such as the vast variability in individual responses to both drugs and herbs. Genetic, environmental, and lifestyle factors play significant roles in how these interactions manifest. Despite the integration of herbs into therapeutic regimens, standardization in herb concentration and purity remains inconsistent, making it challenging to predict interactions accurately.
The current regulatory framework for herbal supplements is less stringent compared to pharmaceuticals, posing another obstacle in understanding drug-herb interactions. Many herbs lack comprehensive clinical trials to evaluate their interactions with medications fully. Therefore, consumers and healthcare professionals often have incomplete information, leading to potential treatment complications. To mitigate these challenges, ongoing research and a collaborative approach among practitioners are essential for improving patient safety and treatment outcomes.
Read Now : “internal Medicine Fellowship Opportunities”
Perspectives on Understanding Drug-Herb Interactions
While formal research plays a key role in understanding drug-herb interactions, anecdotal evidence and traditional wisdom also contribute valuable insights. However, translating these experiences into scientifically validated information remains a complex task. Addressing this requires multi-disciplinary cooperation, drawing on the expertise of botanists, pharmacologists, and clinicians.
To bridge the gap in understanding drug-herb interactions, increased public awareness and education are crucial. Empowering patients to disclose their use of herbal products and fostering open dialogue with healthcare providers can lead to safer and more effective treatment regimens. Furthermore, evolving methodologies in pharmacogenomics and personalized medicine offer promising avenues for elucidating the complexities of drug-herb interactions, potentially transforming the landscape of integrative healthcare.
Evaluating Evidence for Understanding Drug-Herb Interactions
A critical component in understanding drug-herb interactions is evaluating the existing evidence regarding safety and efficacy. Peer-reviewed studies and clinical trials are essential for establishing clear interaction profiles between herbs and conventional medications. However, the lack of high-quality evidence often challenges healthcare providers in making informed decisions regarding concomitant herb-drug use.
To advance understanding drug-herb interactions, it is imperative to encourage more extensive research initiatives and knowledge-sharing within the medical community. Such efforts would help create comprehensive databases and clinical guidelines, equipping practitioners with the tools necessary to make safe clinical judgments and prevent adverse events caused by drug-herb interactions.
Comprehensive Strategies for Understanding Drug-Herb Interactions
Effective strategies for understanding drug-herb interactions involve an integrative approach combining evidence-based medicine and patient-centered care. Cultivating a thorough understanding involves educating healthcare providers on potential interactions, promoting vigilant monitoring systems, and developing risk assessment tools. These actions will ensure enhanced patient safety and optimized treatment outcomes.
A move towards standardized labeling and quality control for herbal products could also aid in understanding drug-herb interactions. By ensuring consumers receive accurate information about the composition and potential interactions of herbal supplements, healthcare professionals can better manage and prevent adverse interactions with prescribed medicines. Through collaborative efforts across multiple disciplines, a more comprehensive understanding of drug-herb interactions can be achieved, ultimately leading to safer healthcare practices.