In the realm of healthcare, understanding drug interaction risks is paramount for ensuring patient safety and efficacy in therapeutic interventions. Drug interactions occur when one drug affects the activity of another drug when both are administered together. These interactions can lead to reduced effectiveness, potential adverse effects, or unexpected increase in drug activity, posing a risk to the patient’s health. Hence, a comprehensive understanding of these interactions is crucial for both healthcare professionals and patients.
Read Now : Heat-induced Cell Death Pathways
The Importance of Understanding Drug Interaction Risks
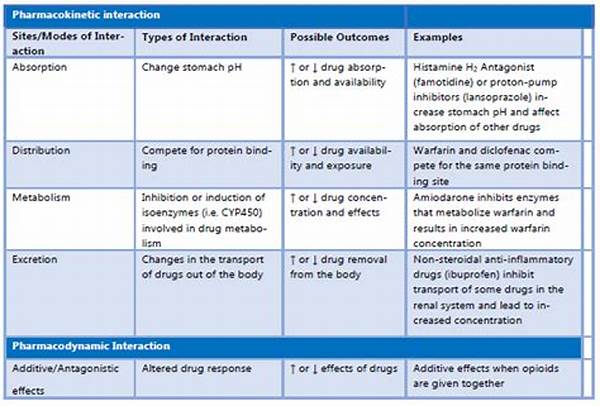
Drug interactions can have profound implications for treatment outcomes. Understanding drug interaction risks is essential because such interactions impact the pharmacokinetics and pharmacodynamics of the drugs. Pharmacokinetics refers to how the body absorbs, distributes, metabolizes, and excretes a drug, whereas pharmacodynamics involves the drug’s effects on the body. When drugs interact, they can alter these processes, resulting in diminished therapeutic effects or increased toxicity. For healthcare professionals, understanding drug interaction risks is crucial for prescribing appropriate medication regimens, adjusting dosages, and scheduling administrations to avoid adverse interactions. Patients, on the other hand, benefit by adhering to medical advice and informing their healthcare providers about all medications they are taking, including over-the-counter drugs and supplements. For instance, certain medications like warfarin, a common anticoagulant, have significant interaction profiles, necessitating close monitoring and an informed approach to co-administered drugs.
Common Types of Drug Interactions
1. Pharmacokinetic Interactions: These involve changes in the absorption, distribution, metabolism, or excretion of a drug, hence understanding drug interaction risks of this type is vital.
2. Pharmacodynamic Interactions: Occur when drugs with similar or opposing effects enhance or counteract each other’s effects.
3. Drug-Dietary Supplement Interactions: Certain supplements can alter drug metabolism, emphasizing the importance of understanding drug interaction risks.
4. Drug-Food Interactions: Food can affect drug absorption; understanding drug interaction risks of this nature is essential in dietary planning with medication schedules.
5. Drug-Alcohol Interactions: Alcohol can dramatically alter the effects of medications, thus understanding drug interaction risks associated with alcohol is vital.
Managing Drug Interaction Risks
Effective management of drug interactions demands a proactive approach characterized by proper patient education, and routine monitoring. Understanding drug interaction risks requires collaboration between healthcare providers and patients. Healthcare providers must remain informed about potential interactions and make informed decisions about prescriptions, while patients should be diligent in communicating their full medication and supplement regimens to their healthcare providers. Furthermore, using resources such as drug interaction checkers and electronic health records can facilitate the identification and management of potential interactions. This collaboration is particularly important in populations with heightened vulnerability to drug interactions, such as the elderly or those with multiple chronic conditions. These groups typically consume multiple medications, increasing the chance of interactions and adverse effects. Hence, understanding drug interaction risks is not only a scientific necessity but also an ethical obligation to prevent harm and ensure optimal pharmacotherapeutic outcomes.
Drug Interaction Risks in Casual Terms
Hey, let’s break it down a bit. Understanding drug interaction risks is like digging the vibes between different meds. When they don’t gel, things get messy, but when they sync, it’s smooth sailing. You gotta be on the lookout because mixing meds ain’t always a breeze. Here’s the lowdown:
1. Meds Party: Some drugs just don’t vibe well together.
2. Eat Your Veggies: Foods can mess with your meds more than you think.
3. Supplements Matter: Even those herbal goodies can clash with your prescriptions.
4. Alcohol Alert: Booze and meds rarely mix well.
Read Now : Deep Breath Relaxation Exercises
5. Timing is Everything: When you take your meds can change the whole game.
6. Age Factor: Older folks usually have more meds to juggle.
7. Check with the Pros: Always keep your docs in the loop.
8. Stay Informed: Use those handy med management apps.
9. Listen Up: Your body gives hints when something’s off.
10. Speak Up: Don’t shy away from asking questions about your meds.
Practical Applications of Understanding Drug Interaction Risks
In clinical practice, understanding drug interaction risks is central to safe and effective patient management. Clinicians often face the challenge of navigating complex medication regimens, especially in patients with multiple comorbidities. Knowledge of drug interaction risks informs decisions regarding medication selection, dosing schedules, and necessary patient monitoring. For instance, a patient might be prescribed a new medication for hypertension, but considerations must be made about existing prescriptions for cholesterol management. Understanding drug interaction risks allows healthcare providers to anticipate potential adverse reactions and adjust treatment plans accordingly. This proactive approach minimizes patient exposure to unnecessary risks while maximizing therapeutic benefits. Additionally, understanding drug interaction risks is critical for those managing chronic conditions, as they often require long-term medication regimens where the likelihood of interactions increases.
Broader Implications of Drug Interaction Risks
Analyzing drug interaction risks extends beyond individual patient care into larger public health considerations. Pharmaceuticals are an integral component of modern healthcare, and their interactions have implications for population health and healthcare systems. Understanding drug interaction risks entails recognizing patterns and trends, such as those revealed by pharmacovigilance data, which help in strategizing public health interventions. For instance, widespread issues with a particular drug combination might prompt more stringent regulatory actions or lead to updates in clinical guidelines. Furthermore, understanding drug interaction risks contributes to the development of new educational initiatives aimed at enhancing public awareness about safe medication practices. On the healthcare system level, reducing adverse drug interactions can curtail the economic burden associated with drug-related complications, thus promoting efficiency and better patient outcomes.
Conclusion: Emphasizing Understanding Drug Interaction Risks
In conclusion, understanding drug interaction risks is an essential aspect of personalized medicine and comprehensive patient care. It involves a multi-layered approach that includes educating healthcare providers, patients, and the broader public about potential risks and strategies for avoidance. Effective management of drug interactions through enhanced understanding, vigilance, and communication can significantly enhance patient safety. Furthermore, understanding drug interaction risks not only improves individual patient outcomes but also supports efforts to optimize public health strategies and healthcare system efficiencies. In an era of increasingly complex pharmacotherapy, prioritizing the awareness and understanding of drug interaction risks is a responsible step towards minimizing harm and maximizing therapeutic potential in medical practice.